Alternative names for amenorrhoea
Amenorrhea
What is amenorrhoea?
Amenorrhoea is the absence of menstrual periods in people who are assigned female at birth during their reproductive years - after the age of puberty but before the typical age of menopause.
Amenorrhoea is classified as either ‘primary’ or ‘secondary’. ‘Primary’ is when menstrual periods have not started by the age of 15 years in the presence of normal growth and secondary sexual characteristics. ‘Secondary’ is the absence of menstrual periods for three or more months if they were previously regular, or for six months or more when they were previously irregular.
It is important to remember that amenorrhoea is normal before puberty, during pregnancy and after the menopause. People may also experience amenorrhoea while breastfeeding - referred to as lactational amenorrhoea.
What causes amenorrhoea?
The most common causes for amenorrhoea can be linked to factors such as recent stress, change in weight, excessive dieting or exercise, or illness.
Other factors causing amenorrhoea include:
- Defects or damage in one or more areas of the reproductive system, such as ovaries, uterus, vagina and parts of the brain regulating reproduction known as the hypothalamus and pituitary gland
- A side-effect from cancer treatment
- Birth control methods, such as the oral contraceptive pill. Even after stopping it may take some time before menstrual periods return.
What are the signs and symptoms of amenorrhoea?
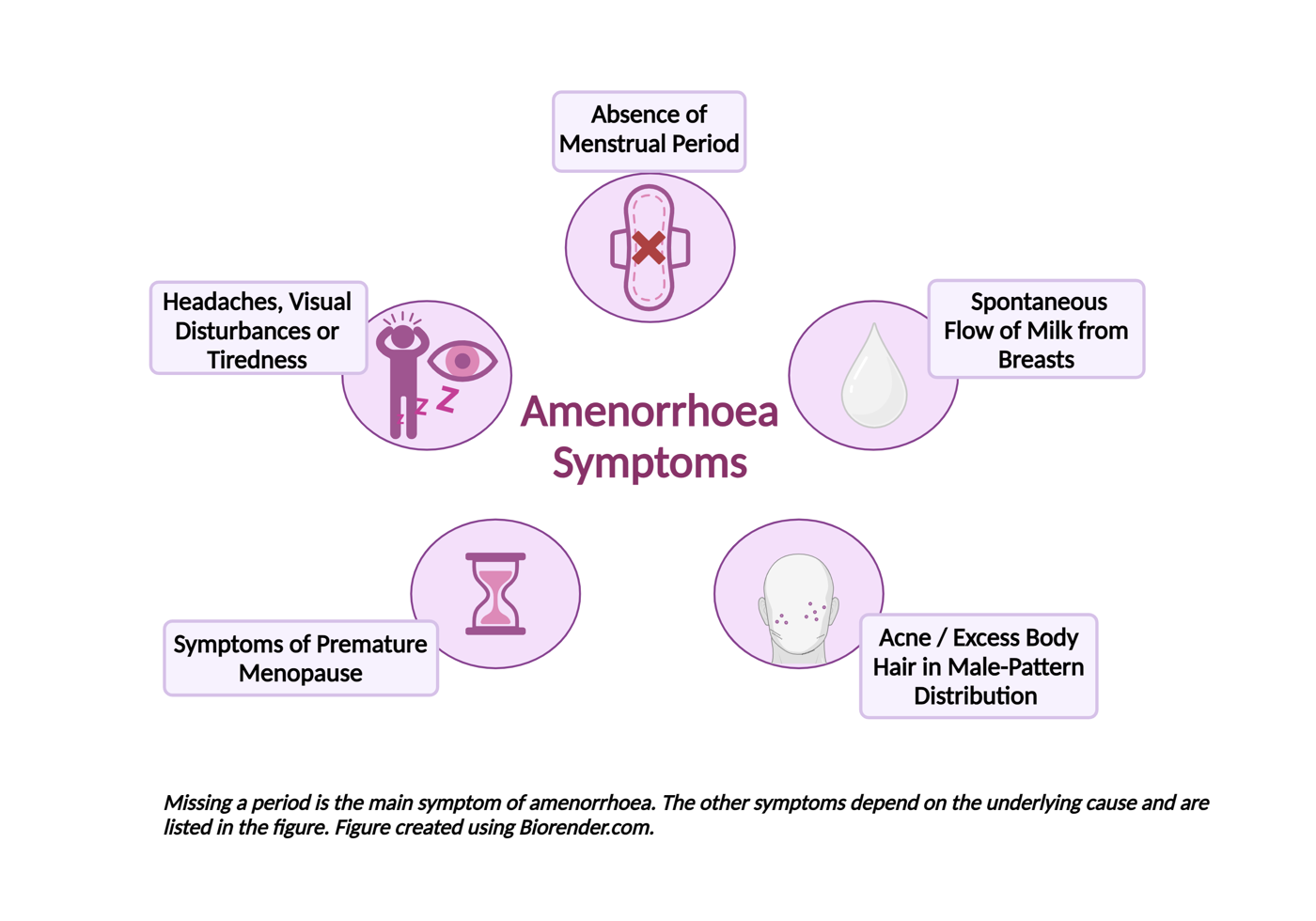
In addition to the absence of menstrual periods, people with amenorrhoea may have one or more of the following symptoms depending on the underlying cause:
- Headaches, visual disturbance or tiredness caused by diseases affecting the hypothalamus and/or pituitary gland.
- Spontaneous flow of milk from the breasts caused by excessive levels of a hormone called prolactin - this is called galactorrhoea.
- Acne and/or excess body hair growing in male-pattern distribution caused by polycystic ovary syndrome.
- Hot flushes, vaginal dryness, poor sleep or reduced libido caused by symptoms of premature menopause known as premature ovarian insufficiency. This happens when the ovaries stop working before the age of 40 years old.
- Short stature and lack of secondary sexual characteristics, such as breast development, if premature ovarian insufficiency is caused by a genetic condition known as Turner syndrome.
How common is amenorrhoea?
Less than 5% of people who are assigned female at birth are affected by amenorrhoea. Secondary amenorrhoea is more common than primary amenorrhoea.
Is amenorrhoea inherited?
The vast majority of amenorrhoea cases are not inherited. However, it is possible that family genetic history may play a role in some cases of primary and secondary amenorrhoea.
How is amenorrhoea diagnosed?
Amenorrhoea is diagnosed based on medical history that shows an absence of menstrual cycles.
A pregnancy test is necessary to rule out pregnancy as the cause of amenorrhoea. Once this has been completed, initial blood tests include measurements of hormones involved in reproduction, such as follicle stimulating hormone, luteinising hormone, oestrogen, prolactin, androgens and thyroid function tests.
In people assigned female at birth who have never had menstrual periods, an ultrasound scan may be performed to look at the uterus, ovaries and the anatomy of the vagina.
Further tests such as a magnetic resonance imaging (MRI) scan of the brain may be performed if medical history or blood tests suggest a hypothalamic or pituitary disease may be the underlying cause of amenorrhoea.
All of these tests can be carried out as an outpatient on a non-urgent basis.
How is amenorrhoea treated?
People affected by amenorrhoea receive counselling to understand the cause and management of their condition, and the potential impact on their fertility. A number of treatments are available for amenorrhoea depending on the underlying cause:
- People who are very underweight through not eating enough or exercising too much often do not have periods; this may be resolved by putting on weight and/or exercising less.
- Surgery and/or medication may be required for pituitary conditions. People with tumours producing excess prolactin, a hormone that stimulates milk production are usually treated with a class of drugs called ‘dopamine agonists’. These drugs reduce prolactin levels.
- Hormone replacement therapy - oestrogen with or without progesterone depending on the underlying cause.
- Prescribing the missing hypothalamic or pituitary hormones that regulate reproduction for people assigned female at birth who want to become pregnant.
- Surgery may be required for people with uterine or vaginal abnormalities dating from birth.
Are there any side-effects to the treatment?
There are a number of side-effects to the treatments available for amenorrhoea. For more information, please see the following articles:
- Prolactinoma - a type of benign pituitary tumour
- Premature ovarian insufficiency - early menopause
- Polycystic ovary syndrome - caused by an imbalance of oestrogen and testosterone
- Congenital adrenal hyperplasia - an inherited condition where abnormalities in the adrenal gland cause low cortisol levels
- Hypothyroidism - an underactive thyroid gland
- Thyrotoxicosis - an excess of thyroid hormones.
What are the longer-term implications of amenorrhoea?
Long-term implications of amenorrhoea often depend on the underlying cause of the condition.
People with amenorrhoea are at risk of developing thin bones and fractures, a condition known as osteoporosis, and therefore should be regularly monitored for bone density. They should also receive counselling and guidance about their fertility if they wish.

